
Knee Replacement Surgery

WHY DO I NEED A
TKR?
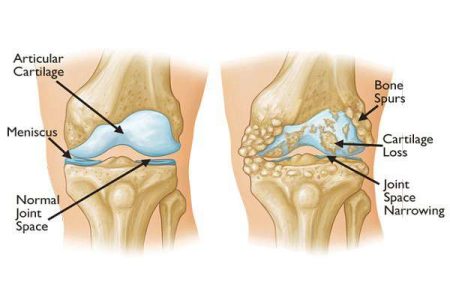
There are many conditions which require a knee replacement. The most common is osteoarthritis. This means that the cartilage of the knee has worn out, resulting in the two bones forming the knee joint (lower end of thigh bone and upper end of the shin bone) rubbing together. This is very painful and stops you being able to move your knee as you once did.
ARE THERE ANY ALTERNATIVES TO A TKR?
Requirement of Knee Replacement Surgery depends upon the severity of your knee arthritis. This option will only be offered to you after other options have been tried and have not relieved your symptoms. This would include medication to relieve the pain, weight loss if necessary, physiotherapy and exercise to reduce stiffness and improve muscle strength and the use of walking aids.

WHAT IS A TKR?
A TKR involves removing a very thin slice (few mms only) of the end of the thigh bone, and the top of the shinbone, and replacing them with artificial knee implants. The artificial knee is usually made of metal alloy such as Cobalt Chrome/Oxinium/Titanium and high density plastic.

Its important to understand that these implants are fitted as caps over your natural knee bones to resurface only a few mm of the worn parts of cartilage and bone. The rest of Knee Bones, Tendon and most ligaments are retained as it is.
HOW WILL A TKR HELP?
The benefits of surgery include:
The majority of patients experience significant pain relief. It is normal to have some temporary discomfort following surgery but our techniques aim to make the surgery as comfortable as possible, in most cases allowing you to walk on the very next day.
The new joint will have highly engineered metal and plastic surfaces designed to allow the joint to move smoothly and freely. The aim would be for you to have less stiffness than before the surgery
With a combination of reduced pain and improvement in stiffness your overall mobility is likely to be improved. This will help you return to a more active lifestyle.
ARE THERE RISKS ASSOCIATED WITH A TKR OPERATION?
As in any operation, there are some risks associated with this operation as well and although rare, it is important that you understand them.
Deep Vein Thrombosis (DVT)
A DVT is a blood clot in the deep veins of the leg. To reduce the risk of developing a DVT, you will be given stockings to help with your circulation and medication that thins the blood. The physiotherapist and nursing staff will show you how to exercise your legs and ensure that you start to move about quickly after your operation. Most people start ambulating on post-op day One thus improving the circulation in the legs and minimizing the chances of getting DVT. You would also be advised to maintain good hydration by taking plenty of oral fluids which further helps in minimizing risk of DVT.
If a clot develops and part of it breaks off, it can travel to the lungs where it is termed a Pulmonary Embolus (PE). This can compromise respiratory function and hence everything is done to prevent DVT from developing.
Infection
There is a small chance (1%) of an infection and all possible precautions are taken to avoid infection during your operation. Mostly it is a superficial infection which can be treated with antibiotics, however, if deep, it may need further washout and change of implants. The redo surgery with the advanced modern technology has a very good success rate.
BEFORE COMING INTO HOSPITAL
Pre-assessment
Shortly before your operation you will be asked to undergo a battery of investigations such as Blood and Urine tests, ECG ECHO and X Rays. You will then see the Anesthetist for PAC (Pre Anesthetic Check Up). May be required to see a physician or cardiologist to check your fitness for surgery. If you are deemed suitable for knee surgery, you will be given the date for surgery.
WHAT WILL HAPPEN WHEN YOU ARRIVE AT HOSPITAL?
You will be admitted to hospital a day before your surgery. Occasionally, it is necessary for patients to have further tests before surgery. On admission, you will be greeted by a member of the team. You will also see several members of the treating team including the anesthetist. If you have any questions, please do not hesitate to ask a member of staff.
THE DAY OF YOUR OPERATION
You will be told not to eat or drink for approximately six hours prior to your operation. The anesthetist will come to see you before your operation. If you are on any regular medication, please ask the anesthetist what you can take on the day of surgery.
The GDA will take you to the operating theatre and a nurse will accompany you and hand you over to the care of the theatre team. The operation is usually carried out under spinal anesthetic and the procedure usually takes approximately 45 minutes to one hour. Including the anesthesia time and positioning plus prepping time you will stay in operation theatre for about 1.5 to 2 hours. You will then be shifted to Surgical ICU for one night.
Your legs will feel numb for few hours after the completion of surgery. This is the normal time required for the effect of anesthetic medicines to wear off. Approximately 2 hours after surgery you will be allowed to have liquids and after 4 hours normal diet will resume. You would be encouraged to do breathing exercises and ankle foot movements. You will meet your attendants after the completion of surgery and once again after few hours.
GETTING BACK ON YOUR FEET
On first post op day, you will be shifted to the ward and the physiotherapist will teach you the first stage of your exercises. They will also help you out of bed and make you walk a few steps with the help of walker. Over the next 5 days you will be taught further exercises, how to walk using appropriate aids and toilet training will be done on commode chair. By the time of discharge our team of physiotherapists will ensure that you achieve independence for activities of daily living such as getting up and about in the house with the help of walker, sitting on chair, using the washroom etc. In normal course you will be discharged home in about 5-6 days.
WHAT HAPPENS AFTER DISCHARGE FROM HOSPITAL
A member of physiotherapy team will attend you at home daily and take you through further exercises to improve the range of motion as well as strength in the knee. Most people need Walker for ambulation for approximately 2 weeks. It is advisable to use high Commode chair or an elevated Toilet Seat for approximately 4 weeks post surgery.
You will be asked to attend OPD after 2 weeks when your knee stitches will be removed and you will get a chance to see the surgeon. Further medications and knee exercises instructions will be given to you. You will be encouraged to start walking with the help of a walking stick. In approximately 4-6 weeks’ time after surgery, most people start walking independently without any walking aid.
EXERCISES
The following self-exercises should be performed three times per day for at least 12 weeks. These exercises will help knee range of motion and strength.
Pain Stiffness and swelling following knee replacement remains for many weeks and is normal for everyone. Take pain killers before you exercise to try and reduce the after
REPEAT FIVE TIMES, THREE TIMES PER DAY.

EXERCISES 1
Sit on a chair with one leg straight in front of you. Place your hand on your thigh just above the knee cap. Lean forward keeping your back straight. Straighten your knee, assisting the stretch with your hands. Hold for approximately 15 seconds.
EXERCISE 2.
Sit on a chair. Pull your toes up, tighten your thigh muscle and straighten your knee. Hold for approximately five seconds and slowly relax your leg.
Repeat 10 times, three times per day.


EXERCISE 3.
Sit on a chair with a towel under one foot. Slide the foot under the chair as far as you can. Move your knee forward keeping the sole of your foot in contact with the floor. Hold for approximately 10 seconds.
Repeat 10 times, three times per day.
EXERCISE 4.
Lie on your back. Bend your leg, place a cushion under your knee. Now straighten your leg by pulling your foot and toes up, tightening your thigh muscle and straightening the knee (keep your knee on the cushion). Hold for approximately five seconds and slowly relax. To make the exercise harder, put a small weight around your ankle.
Repeat 10 times, three times per day.

SITTING
Choose a firm, upright chair, preferably with arms. The ideal height of your chair depends on your height. If your chair is not high enough, have a suitable chair, use firm cushions to raise the height.
When sitting, your knees should be lower than your hips to assist you getting up and out of the chair. Avoid low, soft sofas and armchairs.
To get out of a chair in the early stages when your knee bend is painful, push yourself up on the arms of the chair, taking most of your weight on your un-operated leg. Reverse the procedure to sit down. If you have had both knees done get someone to give you support in the armpits at the time of getting up and sitting down on the seat.
Use the same method to get on/off the toilet.
KNEELING
Kneeling is not advisable for several months following your operation, after which, you may kneel down as you feel able. You may find it more comfortable to kneel on a pad or cushion.
Many patients find they cannot kneel after their operation either because it is uncomfortable or because they are experiencing a strange sensation. You must take this into consideration if you kneel a lot due to your work or hobbies.
DRESSING
Dress sitting on a chair or the bed. It is easier to dress your operated leg first and undress it last. It is advisable to wear good supportive shoes with low heels (you may find slip-on shoes easier to manage).
HOUSEHOLD TASKS
To start with try and do most tasks in sitting position. A high stool is useful so that you can still reach the worktops. If you are unable to carry items, a kitchen trolley may be helpful. For 4-6 weeks after your operation you are likely to need help from your spouse, relatives or friends for household activities.
GETTING IN AND OUT OF A CAR
The passenger seat should be as far back as possible and slightly reclined. If needed use a small cushion to make the seat level. With the passenger door open, back up to the car until you feel the seat at the back of your knees and gently lower yourself down. Lift your bottom back towards the driver’s seat to give you plenty of room to swing your legs in. To get out of the car, reverse the above procedure.
DRIVING AND RETURN TO WORK
This varies from person to person and largely depends on their fitness levels. Nevertheless, most people resume driving between 6 to 8 weeks and can return to work between 8 to 12 weeks, but this also depends on the nature of your work and how you usually get there.
WHAT SYMPTOMS ARE CONSIDERED NORMAL AFTER TKR SURGERY
Temporary swelling and stiffness around the knee, especially after rest, are normal following a knee replacement and can persist for as long as 6 to 8 months after surgery. These are harmless and a part of natural healing process. In order to counteract these, try and always sit with your legs/feet elevated and move your knee through range of motion before getting up after having sat for a period of time. Do not stand in one position for long as gravity will make your knee swell even more.
Numbness over the outer half of knee and clicking sound on walking is also quite common. Again this is normal and you need not worry about this.
Feeling tired and exhausted easily is also common for few months after surgery. This is normal and your strength will gradually return over the next few months.
Some people can have disturbed night sleep for a period of time. You need not worry for such symptoms as they disappear spontaneously in almost all patients allowing them to lead a pain free happy life.




